Measuring our bodies against the reluctant microbiome metaphor
1.
A few months ago I had my gut microbiome analyzed--a $99 value--free of charge. The American Gastroenterology Association made the offer to all of its trainee members, myself included. Through the mail I received two cotton swabs in a sterile plastic tube (the accompanying instructions were careful to specify that the amount of stool needed for a successful analysis was likely less than I expected). I sent back the swabs, no longer sterile, and a few weeks later looked up my results online.
As a gastroenterology fellow, I hear a fair bit about the microbiome--a term referring to the aggregate genetic material of the microorganisms that colonize our bodies’ various surfaces--as a vast new frontier for biomedicine. In general, I try to maintain some skepticism about the whole thing. The science is exciting but young: studies of gut flora tend to yield associative rather than causative conclusions, and the results of most animal studies are often hard to reproduce in humans. Experimental techniques vary by laboratory, and the best methods for storing and culturing samples are matters of ongoing debate. Conventionally undetectable bacterial species, so-called “microbial dark matter,” and innumerable ambient viruses in the gastrointestinal tract constitute a large set of potentially confounding variables.
All the same, when my personalized readout became available, I scrutinized it at length, working to discern my bill of health from a smear of stool at a single point in time. There was a bar graph comparing my dominant bacterial subclasses with those of other participants matched to me by age and gender. Heat maps and scatter plots triangulated the composition of my microbiome with that of other Americans and, by way of cultural contrast, a cohort of Malawians. My sample, I was told, contained at least ten rare taxa, the names of which pleased me, though I had never heard them before--Dorea, Dermabacter, Anaerofustis.
Funhouse mirrors are still mirrors, prone to catching the eye. Knowing full well the limits of these metrics, I found myself reading through the latest journal articles for a sense of what the results might mean for me and my body--functional for now, but charged over the last few years by every passing ache or pain with a sense of its pending brokenness.
2.
In theorizing about our health, humans have a longstanding habit of mapping our bodies to the wider world. This pattern runs through a variety of healing systems as a string of what certain historians of medicine have called “microcosm/macrocosm homologies”--explanatory parallels between small and large spaces. Physical regulation is compared with the political state in ancient Chinese writing, for instance, and with the cosmos in Ayurvedic texts. In 16th century Europe, the scholar Paracelsus attributed anatomically specific illnesses to toxins emitted by celestial forms--the spleen was poisoned by Saturn, the liver by Jupiter, the brain by the moon. He further postulated that the affected organs could be restored to health by plants that bore them visual resemblance.
The symbolic underpinnings of the modern microbiome concept are similarly arranged. The gut, in particular, is host to a collection of organisms commensurate in number and complexity with a world in itself; and recent studies have accorded these organisms with progressive influence over our physical and mental wellbeing. The resulting biological model figures the human body as an intermediary between the microcosm it contains and the macrocosm it inhabits.
Both realms are subject to similar threats--a loss of biodiversity attributable to our own behavior. Doubt has fallen over a range of contemporary practices shown to disrupt the composition of our microbiota, ranging from the overuse of antibiotics, to the frequency of C-sections, to the low-fiber, high-fat diet shorthanded as “Westernized.” Intuitively, these practices seem to correlate with much more visible ravages of civilization on the global landscape--longstanding environmental challenges like pollution and climate change, the worsening of which appears to be increasingly and grimly certain.
This explicit mapping between inner and outer worlds has helped establish new priorities within the modern biomedical mission. Public health advocates like Martin Blaser, a pioneering microbiologist and former chair of medicine at NYU, often utilize this analogy in calls for a more scrupulous approach to clinical intervention. Blaser’s 2014 book, Missing Microbes, connects different types of environmental instabilities to build the case for a novel understanding of sickness and health. “I see many parallels between our changing climate and our changing resident microbes,” he writes, speculating on the increasing prevalence of diseases like asthma and obesity. “Like the worsening hurricane seasons we are seeing, these outcomes are bad enough, but they are also indicators of our larger imbalances, the loss of our reserves.”
This notion of balance is a longstanding feature of medical thinking, from classical formulations of humoral theory to contemporary models of biochemical homeostasis. As such, an understanding of health as a consequence of maintaining the right parts in the right proportions--whether phlegm and bile or Firmicutes and Bacteroidetes--comes with deep-seated narrative appeal. And yet, the mechanism of disease implied by the microbiome model is also one particularly well suited to the contemporary moment. It provides a new mode of expressing an old distress, transforming the unease with which we regard our effects on the natural world into a literally visceral phenomenon.
Balance is likewise a core metaphor for the modern environmental movement, latent in the conceptual understanding of ecosystems and sustainability. Analogous threats breed analogous anxieties, in light of which our contemporary fascination with the microbiome seems distinctly Anthropocenic--belonging to this putative geological age defined by human activity. We’ve taken the world, as we’ve lately come to see it, into ourselves--depleted, worn away, eaten up.
3.
The ecological analogy is often justified. Microbiome research consists of explicitly transdisciplinary questions, and the importation of tools from the environmental sciences is to some extent obligatory. Like any complicated idea, though, the microbiome is defined by its boldest outlines when distilled for popular consumption.
How might this framing fail us? To the extent that descriptive parallels set the stage for moral ones, the gaps left by science are well positioned to be filled by sentiment. Mapping our bodies to an endangered world has a way of skewing the biomedical dialogue toward stock ecological narratives in which the trappings of civilization are inherently destructive, or the most valuable landscape is the one least shaped by human hands.
In this regard, the reparative spirit that has emerged in the public sphere with respect to the microbiome seems pre-loaded with a sense of culpability. Recently published self-help books on gut health favor a rhetoric of loss and rehabilitation in their service as guides to, for example, “restore your inner ecology.” Coursing beneath this nostalgia for times past is a subtle sort of primitivism, the knee-jerk tendency to view indigenous cultures as time capsules for physical vigor that civilization has elsewhere degraded. Data suggest that microbial diversity is often higher in remote populations, but the health implications of this difference remain conjectural. Even so, the idea was credible enough to inspire at least one independent researcher to introduce the stool of a Tanzanian hunter-gatherer into his own rectum with a turkey baster.
A wounded ecological reading of the microbiome is not inevitable. Science journalist Ed Yong’s book, I Contain Multitudes, published this past August, is an overview for general audiences that favors a tone of wonder over warning. It does so in large part by emphasizing the insignificance of humanity relative to bacteria in evolutionary history. For example, in response to the idea of the Anthropocene, Yong writes, “You could equally argue that we are still living in the Microbiocene: a period that started at the dawn of life itself and will continue to its very end.” While acknowledging our real capacity to damage microbial ecosystems beyond repair, the author humbles himself repeatedly to those ecosystems’ complexity and resilience. Whereas Blaser’s analysis functions as an alarm call, Yong’s is rendered as a celebration of biological peculiarity, all that we don’t yet know.
Macro-environmental theory, for its part, has matured beyond the tidy concept of unspoiled wilderness. Contemporary ecocritics argue that stasis is a false ideal, deployed primarily for aesthetic effect; it represents a contrivance of “pastoral ecology,” a quaint and outmoded view of nature typified by a harmonious resting state. As such, distinctions between human and non-human worlds may be viewed as increasingly arbitrary with respect to the primary goal of safeguarding both. Peter Kareiva, former chief scientist at The Nature Conservancy, a well-known charitable organization, has provocatively suggested that modern environmentalism would do well to relinquish the old metaphors of a fallen world and embrace a more durable understanding of nature. Granting the world some buoyancy in the face of human enterprise, he maintains, will allow us to develop more creative, inclusive, and potent solutions as its stewards moving forward.
Recognizing that this stance is controversial with respect to the planet’s shared spaces, it seems considerably less problematic when applied to the space of a single colon. Without diminishing in any way the urgency of the larger conservationist movement or the startling irresponsibility of its dismissal, it should be noted that there are differences between these two types of environments. Unlike rainforests or coral reefs, my body is just over thirty years old and is mine to steward alone. Microbes connect us vertically across generations and horizontally with every handshake, but the world inside me--however balanced, diverse, or protected--is fated to collapse whenever I do.
4.
Individual profiles of the microbiome may yet mature into meaningful portraits. Despite the continued relevance of an eye-rolling award regularly given out by evolutionary biologist Jonathan Eisen for “Overselling the Microbiome,” the field tends to be savvy to its own limitations. Recognizing that bacterial diversity is a moving target, researchers have become more attentive to obtaining multiple samples over time, despite the extra costs of this approach. Interest in the relative abundance of species is coupled with progressive interest in their associated metabolome, the collection of biologically active molecules that those species produce. In general, methods such as these work toward establishing a more nuanced understanding of the relationship between microorganisms and human health.
At the same time, the unfinished quality of microbiome science has not precluded attempts to commodify it. Start-ups built around microbial therapies have surged in value on the basis of hype, and some have already crashed upon failure to deliver. The scale and enthusiasm of these ventures seem driven as much by the scientific potential of the microbiome as by the affective power of its conceptual model. There is a clear imperative to invest, both financially and emotionally, in the future of this microcosm.
For now, publicly available microbial analyses are like Rorschach blots, reliant on the viewer for active interpretation. The tone of many readings tends toward penitence: in parallel with ecological convention, we are poised to see our civilized guts as reflective of descent from an earlier, healthier, more natural state of being. So far, these little landscapes have struck us as more fragile than plastic, but the basis for this outlook at a planetary scale does not necessarily hold firm at an intestinal one. With respect to the microbiome, recognizing the sentimental parameters of this particular homology can help enlarge our therapeutic vision and bring it, at least partially, under our control.
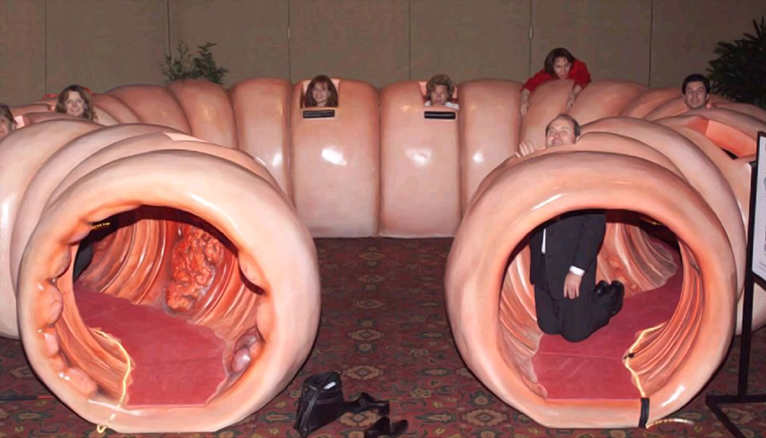
I’ve been asked by patients with all sorts of symptoms if they might be considered for a stool transplant--the instillation of fecal microbiota from a healthy donor into the bowels of an unwell recipient (but with a colonoscope instead of a turkey baster). The formal diagnoses for which this procedure has been studied and approved are in fact quite limited. In some corners of the public consciousness, though, the idea of resetting one’s intestinal bacteria has taken on the dimensions of panacea. Prelapsarian ideals of personal and environmental health are perhaps subject to similar charges of romanticism and naiveté, and I readily confess to finding them quite charming myself. The impulse they draw upon, after all, is reflexive and tenderhearted--to replant the garden, to start over again.