By Deanna Day
When Mary Putnam Jacobi was a girl in New York, it was an established scientific fact that women’s bodies were vulnerable; that is, more vulnerable than the bodies of men. In the early 19th century, everyone knew that women’s bodies were weaker, more susceptible to disease, and plagued by the influence of their emotions. The biggest liability of all was their menstrual cycles.
In the 1800s, menstruation was a process that (mostly male) scientists understood as unpredictable, debilitating, and dangerous. But—like many of the beliefs held by men about women’s bodies during the 19th century—both the empirical and theoretical bases of these claims rested on epistemological foundations that were being eroded by new technologies, new techniques, and new people wielding them.
Despite these prevailing attitudes about women’s bodies—which were used to justify excluding women from all kinds of supposedly taxing activities, including elite occupations—Mary Putnam Jacobi became one of the first women to rise to prominence in the medical profession. During Jacobi’s lifetime, simply being a woman in medicine was a feat of some activism. But Jacobi went a step further, making women’s rights the subject of both her political efforts and her scientific research. By conducting research focused specifically on menstruation, Jacobi took the entire medical profession to task for treating women’s bodies as inherently pathological.
In an observation that foreshadows 20th century feminist theory, Jacobi noted that men’s bodies were treated as if their reproductive health and sexual expression were, within wide parameters, neutral to the point of being “unsexed.” By contrast, women’s reproductive systems were treated as if in every case they were complicated, fragile, finicky, and liable to deteriorate at any moment. In other words, women were marked by their biology. Women had a biological sex that must be monitored and coddled. Men, by contrast, were practically without biological sex. Men were generically human, in need of no special consideration. Men simply…were.
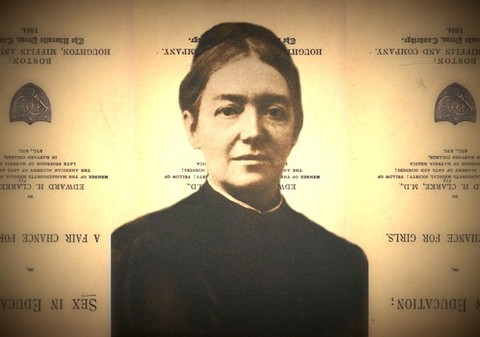
In 1873, during Jacobi’s first year as a professor at the Women's Medical College of the New York Infirmary for Women and Children, Harvard physician Edward H. Clarke published a book that set off a transatlantic debate about women’s abilities to handle advanced education. In Sex in Education; or, A Fair Chance for the Girls, Clarke argued that subjecting women to higher education—especially in programs where women would be educated alongside men—would place such an undue burden on women’s physiology that they would become gravely ill, even to the point of lifelong sterility.
Jacobi’s response to this argument was to make the study of menstruation one of her first major research projects as a professor. Jacobi’s goal was clear and explicit: to disprove the idea that menstruation was a debilitating condition for women.
Not only was this research goal radical in its own right, but so too were the tools that Jacobi used to achieve it: quantitative data collection and statistical analysis. Jacobi distributed approximately a thousand survey tables, which asked women sixteen questions about their health, education, menstrual cycles, and physical abilities. From these, 268 women responded. They provided Jacobi with enough information to fill 24 separate tables of comparative data, which she used as a foundation to prove that women experienced no systematic or predictable debility during menstruation.
When Jacobi enrolled women into her medical research studies as active participants, she made them into medical workers. Her precedent would become a model used over and over for more than a century as medical researchers recognized women as ideal data-gatherers—they knew their own bodies, they were increasingly educated and able to follow instructions, and their labor was free.
Today, quantitative data collection and statistical analysis are generally accepted principles of scientific research; so accepted, in fact, that data and science are often used as almost interchangeable terms. But during the late 19th century, this approach to scientific discovery was still relatively new. Early data-collecting tools like thermometers and sphygmomanometers had only recently been introduced to medicine, and some physicians were resistant to tools they thought might usurp even a small amount of their expertise or authority. Many physicians, like the aforementioned Dr. Clarke, based their medical opinions and treatments on the more anecdotal method of examining individual case studies and comparing them to their previous clinical experiences.
When Jacobi finalized her menstruation research, in an essay titled The Question of Rest During Menstruation, she submitted it to Harvard University for consideration for its prestigious Boyslton Prize. Given the controversy that surrounded its subject matter and the fact that her own reputation preceded her, her advisor recommended she submit the essay under a pseudonym. She chose the Latin phrase Veritas poemate verior, “a truth truer than a poem.” Based on a statistical analysis of quantitative data, she believed that her argument was more convincing—more truthful—than scientific claims based on poetic ideas of femininity or women’s inherent frailty.
For Jacobi, and the generations of women who followed, physiological data was to become as truthful an expression of their bodies as their lived experience within it. The two have become indistinguishable after decades of immersion in a medical system that has asked women to keep symptom logs to track everything from menstruation and blood pressure to weight loss, cold and flu symptoms, and blood sugar levels.
Yet, despite Jacobi’s own narratives of self-evident data, and the critical goal they served, quantitative data does not simply exist in the world, waiting to be scooped up and dropped into a table. Data is the end of a process, not the beginning of one.
Data production is always difficult—the world that scientists observe is never stable, so researchers have to make a choice about which moment to crystallize in a data point. Instruments can be finicky, producing different readouts at different times for reasons that may not be understandable. In medicine, data production has an additional degree of difficulty: medical research subjects aren’t merely extant phenomena to be observed, they’re people with individual experiences, as well as foibles (like physical needs or faulty memories) that will always interrupt any data gathering protocol, even (maybe especially) if they are themselves the ones implementing it.
The history of data is the history of labor, and the history of labor is the history of women’s labor. Because women’s individual experiences are so often reduced to the particular, and the particular so often dismissed as the unimportant, translating ourselves into the form of collective data has often meant gaining recognition in the eyes of a medical authority that is incapable of seeing us in any other way. At the same time, making ourselves legible has also involved taking on the burden of data creation: monitoring ourselves, recording ourselves, and even modifying ourselves to massage “better” data for our doctors.
Women’s bodies are both the raw material of medical research and one of the agents of its production. The data that we make is both a product and a tool, a thing we make and a thing that makes us. Data isn’t truth, but language. It can help us decide or express the truth, but data never is the truth.
Further Reading
Carla Bittel, Mary Putnam Jacobi and the Politics of Medicine in Nineteenth-Century America (Chapel Hill, NC: University of North Carolina Press, 2009)
Lisa Gitelman, ed., “Raw Data” is an Oxymoron (Cambridge, MA: MIT Press, 2013)
Deanna is research fellow in the Center for Applied History at the Chemical Heritage Foundation. She is currently writing a book about the thermometer’s history in American medicine, showing how it laid the intellectual and material foundations for our current approach to self-tracking technologies.
Contact: deannaday.net; @deannaday