Western psychiatry pathologizes and depoliticizes the trauma experienced by refugees
Contemporary psychiatric care and infrastructure in the Middle East is inadequate to the occurrence of psychiatric conditions resulting from armed conflict, military occupation, persecution and displacement. Western countries make nominal efforts towards closing this gap, exporting psychiatric treatment and medication globally—including to the Middle East, where it is often used in the aftermath of conflict—but this is structurally undermined by continuing Western military intervention and arms trade in the region as a contributory cause of these psychiatric conditions.
Though there have historically been flows of migrants and refugees from places of conflict in the Middle East to Europe, these issues in psychiatry are increasingly pertinent with the scale and speed of the recent influx of refugees in the so-called "European migrant crisis." The already limited infrastructures for Transcultural Psychiatry in the west — an approach that foregrounds how differences in sociocultural norms are implicit in criteria for psychiatric diagnoses, and how these norms marginalize cultural and ethnic minorities —may be equally unable to cater to the specific needs of increasing refugee populations, both in terms of psychiatric help and the linguistic and cultural support in administering it. Nevertheless, refugees arrive, and the majority need some form of psychiatric care in the short or long-term.
PTSD is a particularly common condition for refugees. Post-Traumatic Stress Disorder occurs when exposure to a traumatic event has continued effects even after the initial threat has subsided, with symptoms including hypervigilance and flashbacks; it alters biological reactions to stimuli, perceiving everyday audio-visual phenomena as a "threat." Many symptoms overlap between psychiatric conditions, and refugees can have multiple conditions (e.g: PTSD, anxiety, depression). Though these conditions are not necessarily permanent, as seen by a growing body of research into "neuroplasticity" and brain flexibility, they can still have lasting or permanent effects on peoples’ lives.
In order to "diagnose" psychiatric conditions, a person's experiences and biomedical information must be quantified and abstracted, their body medicalized and objectified. Many critics of Psychiatry have argued for a shift from the biomedical, individual and familial models of mental health to looking at a wider socio-political context; from a reformist idea of adaptation (e.g: that we should be more "aware" of mental illness,) to looking at its potential structural causes.
However, the process of diagnosis is required for the individual to be able to access psychiatric services; for example, in the UK, general practitioners, (GPs), are the gate-keepers to more specialized psychiatric care. GPs often provide self-report questionnaires for anxiety and depression, which depend on the patient being able to identify and articulate their emotional experiences, and whether these are translatable into diagnostic criteria. These results effect benefits and employment, as the state measures, tests and attempts to control their "fitness for work" and "productivity"; mental illness becomes a venue for biopolitical control of the individual. Increasingly, however, because of austerity policies, it has become the responsibility of individuals to practice their own self-regulation.
As a user of psychiatric services in London, I saw a great inequality in services and resources between the different boroughs of the city, and within this further differentiation of approaches and diagnoses with each doctor. Access to psychiatric health-care exists in a double bind: if one has a debilitating illness (that prevents them from leaving the house such as social anxiety, dgoraphobia, catatonic depression) then they will be unlikely to attend appointments with a GP or psychiatrist to get medication and treatment, or access other state services they are entitled to such as disability benefits. In 2010, the Conservative government implemented policies to reduce low-income and disability benefits, where an estimated sixty people died directly related to benefits withdrawal between February 2012 and the 21st of October 2014; based on information provided by disability rights group Black Triangle, a third of these people had pre-existing mental health conditions and two-thirds were driven to suicide. The Black Triangle’s "UK Welfare Reform Deaths" campaign, which coincided with Department of Work and Pensions internal investigations, led to a UN investigation into the UK’s failure to meet its disability rights obligations.
In mainstream British media, psychiatric conditions are often considered an "invisible illness," at least when the person is not having an acute episode of psychosis, mania, or other recognized forms of "abnormal" behavior. This could be seen as a comparative privilege (in terms of passing as privilege), as individuals may have relative choice whether to out themselves in various contexts; though people with psychiatric conditions are often marginalized, their experiences of prejudice and inequality may be decentered and delegitimized by their ability to "pass." There continues to be polarity in healthcare available by income and workplace discrimination. And when it comes to minority populations and refugees, these problems of varied treatment and gatekeeping become deepened by cultural difference, language barriers, and racism.
There are disproportionately high rates of psychosis and schizophrenia in Black minorities in London, where a disproportionately high percentage also live in poverty. Despite this, there is comparatively little psychiatric research into minority communities, and where it exists there is little translation of this into longer-term government policy; specialist psychiatric care for ethnic minorities is often provided through short to medium-term funded research projects and charities, but often only where there is a population threshold in the borough. There is a tendency to misdiagnose signs of distress as psychosis or schizophrenia where it may be a proportionate response to life circumstances such as poverty and racism, particularly with cultural differences in how this distress is expressed. Psychiatric research, as part of wider scientific research, assumes there are universal scientific laws, and that such research is a common language that is cross-cultural. Whilst linguistic translators are provided for psychiatric research on minority groups, this does not necessarily "translate" cultural difference; for example, in some cultures people may not identify individualized emotions but identify them as part of collective, family or social feelings, which are not compatible with psychiatric diagnoses.
While working as a psychiatrist in French-colonized Algeria, Frantz Fanon in 1961 explored how the internalization of a colonized subjecthood by the population had dehumanizing effects that impacted their mental health. Roland Littlewood noted the incidence of marginalized groups that have high rates of schizophrenia, which tends to occur globally in circumstances of colonization; many minority groups in the UK formed after the British colonization of their home countries, and subsequent flows of migrants and refugees have continued since then. Littlewood suggests that a specific neuropsychological relationship exists in the use of dominant colonial language "in which you yourself are objectified" and "alienated by your very process of thought," that can lead to behaviors and expressions that may be perceived as psychopathologies. Fanon was writing about psychiatry within a modern nation-state and at the beginnings of post-colonial ideology; this has since developed since into a globalized, marketized psychiatric care system.
If research into psychiatric conditions of non-white minorities within Western nations is poor, there is perhaps an even greater lack of Psychiatric research into trauma and PTSD in Arab populations residing in the Middle East, especially considering the rate of recent and continuing conflict in certain parts of the region. The study of PTSD in psychiatry usually depends on state and private funding for research, and so has tended to focus on drone pilots and Western and Israeli military. As modes of funding for research, policy and care are still state-based, in the Middle East, where many borders are re-drawn and contested and populations migrate with conflict, it can be even harder to administer services for these populations. During conflict, health care and psychiatry are considered global humanitarian issues by the United Nations, rather than issues of the individual states; however, this often results in a series of temporary responses rather than longer-term systematic ones. There are many complexities in treating PTSD that are not accounted for in the short-termism of healthcare provision and public policy; for example there are delays between the onset of disorders and onset of treatment, and cases of indirect as well as direct trauma, such as children seeing events on television or hearing of killings through adults. The effects of trauma can be lifelong, as well as intergenerational, where longer-term research and healthcare planning is needed to address these issues.
However, in the context of military conflict, could we see trauma not as a disorder or individual pathology, but a wholly proportionate reaction to the socio-political context?
• • •
According to the UNCHR (UN Refugee Council) 2015 has seen a 20-year high in the global total of refugee applications. Figures from the UNHCR in 2014 show that Syria, Iraq, and Afghanistan have the highest percentages of applications for asylum in industrialized countries; this article will be focused on Syrian refugees. It’s important to note that, while news of this refugee crisis focuses on those headed to Europe, whenever there is a conflict in the Middle East most refugees stay in the region. In August 2015, the UNHCR made an estimate based on data from 2014 that there were 119,891 applications from people from Syria applying for asylum in EU states (28 countries), and 146,373 applications to wider Europe (38 countries).By comparison, there are 4 million registered Syrian refugees in neighboring countries, including 1.94 million in Turkey, 1.1 million in Lebanon, (despite the country not being party to the 1951 Refugee Convention,) 629,266 in Jordan and 249,463 in Iraq; all of these countries have lower GDPs than Western Europe. This puts the apparent "crisis" of Europe’s infrastructural capacity in stark relief.
The overall number of refugees seeking asylum in industrialized countries has increased, but government responses to this increase have depended on how it has been framed in national political discourse. Since the 1990s, and more so since 9/11, there has been an increasing language and proliferation of government and NGO organizations based around security; this is also seen in attitudes towards asylum and migration. Migration has increasingly been seen as a process that needs to be controlled, with political parties mobilizing a politics of fear, positioning migrants and refugees as an existential threat to the nation-state, despite the acceleration and deepening of transnational ties via globalization. This is exacerbated by political parties diverting anxiety about such issues of globalized capital towards migrants groups instead.
The problematization of movements of people in terms of legitimacy and crisis is formed by popular opinion and news media – which both respond to and inform political rhetoric. It is this construction of illegitimacy that perpetuates the idea of crisis, even when there is no such thing as an illegitimate refugee or asylum seeker, as they are protected by international law.
Even with this rhetoric of crisis and urgency, the UK government’s response to the situation has been relatively small, given that the military conflict in Syria has been on-going since 2011 and Britain has supported direct military intervention. In the apparent generosity of the UK recently deciding to take in Syrian refugees — which they are legally obliged to do, as they co-wrote and signed the 1951 UN Convention — there has been a collective forgetting of previous flows of migrants, like those from the Balkans in the early 1990s, and of the selective generosity in accepting refugee populations after the Second World War in 1945. Even when refugees do receive asylum, it is limited; for example, the UK accepts refugee children, but they then have to leave when they are 18, or have to prove to the Home Office in court that they have substantial ties to the UK. Though the UK government has just announced an official policy to invest in rehousing Syrian refugees, general austerity measures have reduced the capacity of informal, civil-society organizations that historically provided services to asylum-seekers and refugees. For example, in London the Refugee Council of Lambeth and Southwark that helped those seeking asylum closed on 1st April 2014 as the Home Office transferred services to the larger charity Migrant Help.
The UK government claims it does not have the resources to handle this influx of refugees, yet by comparison to how much was spent by the UK government in military intervention in Syria, Iraq, Afghanistan, they could easily afford to. It was estimated that between 2003-2009 the UK spent £8.4 billion on the Iraq war, and at least £37 billion in Afghanistan between 2001-2013. The UK Ministry of Defense gives a lower estimate of £25 billion, but this does not account for the total costs of the war including long-term care for returning soldiers with physical injuries and PTSD. The UK spent approximately £79 million on military intervention in the Syrian civil war so far, and it is now clear that the 2003 invasion of Iraq contributed to the formation of ISIS, which is provoking the movement of refugees in the first place.
Since 2012, the UK has allocated £1 billion to partner organizations including UN agencies, NGOs and the Red Cross, as well as donating to refugee camps in the Middle East and will spend £1 billion on housing and living costs of refugees entering the UK, but for only up to one year of their stay. In comparison to ongoing total military spending in the region and intended UK military intervention, these efforts are minimal. When it comes to access to natural resources and geopolitical power, there is a great deal of investment and diplomacy, but the human fallout from military intervention is given much lower priority.
• • •
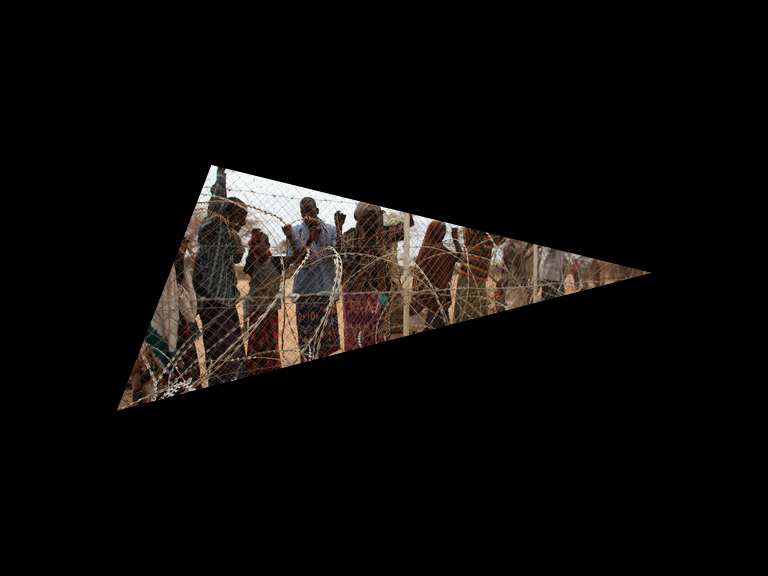
Of the refugees fleeing conflict, it is likely a large number have psychiatric conditions from their experiences of conflict or of seeing people die in the process of traveling to Europe. As there is uncertainty of the refugees’ end destination, many governments cannot plan in the medium to long term for psychiatric healthcare for these groups, and governments do not want to make substantial investments into services within refugee camps that they prefer to see as temporary, and where the staff are on short-term staff contracts. There is little transitional or sustainable healthcare as refugees move between camps to their destination country. There are also psychological impacts of living in refugee camps themselves, in their isolation, and infrequent or lack of interaction with the outside world and their former support networks; bureaucratic processes of applying for asylum can take months, with no certainty, which can further lead to a sense of apathy and clinical Depression.
In Lebanon, in the refugee camps for Palestinian refugees it is estimated that a high proportion of those living in the camps suffer from psychiatric conditions, and the numbers have increased massively with the influx of Syrian refugees, the majority of whom are young and likely to suffer from PTSD. Only 12 percent of Syrian refugees across the region live in formal refugee camps, and can thus access formal psychiatric services. In refugee camps in Iraq, doctors are seeing not only an increase in the rate of psychiatric conditions but also more complex reactions and symptoms, and increased rates of extreme conditions such as schizophrenia. Increasingly, Palestinian refugees within Syria are internally displaced or stranded, as Jordan closed its borders to Palestinian refugees early in the conflict in 2011, and Lebanon closed its borders in May 2014.
The problems of psychiatric treatment within refugee camps reflect the wider problems of lack of resources in refugee camps generally. According to Charles Watters, the term "PTSD" is often used to flatten different kinds of reactions to trauma into one overarching category. Still, the use of the term is effective as a means to get funding, and so rates of PTSD in refugee camp populations are often overestimated for pragmatic reasons. The social construction of refugees and asylums seekers in this psychiatric context as "pathological" individuals can impact their self-perception; they are often treated as passive victims rather than being allowed agency to assert their own interpretations of their needs and choices for treatment.
Psychiatric care is only beneficial if included as part of wider holistic care in refugee camps, and few camps include bottom-up approaches of asking refugees what would help them; when refugees are asked and answer, they more often point to socioeconomic factors than a need for psychotherapy, though these are interconnected. The mental health of refugees is seen to be better where they are allowed to retain their own cultural identity and support networks, building their resilience and ability to adapt to new circumstances; having current or former-refugees help providing services themselves is also beneficial for a sense of self-help and community support. Where formal psychiatric care may not be available, other grassroots alternatives may form with facilitation by charities and NGOs, forming a sense of self-empowerment and agency. Though scarce food supplies in refugee camps lead to physical and mental exhaustion, where a sustainable support network may not be able to grow, and with the uncertainty of being moved at any time people may not be willing to make such an investment to root themselves in the camps.
The current refugee "crisis" is symptomatic of wider longer-term structural problems in the Middle East, in which Western intervention continues to play a large part. Though it would be reductive and over-deterministic to reduce current events in the Middle East to the history of Western intervention alone, the legacies of military intervention, redrawing borders, and supporting regimes that fulfill short-term goals of Western governments instead of those that would be beneficial in the long-term for the region has contributed to continued instability. The idea of Western-exported psychiatry as a cure to mental health "problems" in a large part both caused (in terms of military intervention) and ideologically constructed (in terms of individual pathology) by the West itself is fundamentally contradictory. Ongoing military intervention reduces the infrastructural capacity for indigenous forms of mental health care to grow and develop, and there are ethical questions surrounding the export of Western-modelled psychiatric care as one facet of a continuing neo-colonial project.
There remains a great lack of self-reflexivity in and by the West as to the impacts of its (neo)colonial violence, in terms of its responsibilities in contributing to the current refugee "crisis" and falling short of providing a proportionate amount of aid in response. This is part of a wider lack of acknowledgement of sociopolitical inequalities and psychological damage of colonial violence, both in ethnic minority communities within the UK and on a global scale in former colonized countries. Partial, Western-centered psychiatric care for individuals’ symptoms both obscure and reproduce wider structural problems.
However, in the face of this, alliances can be formed where these different kinds of inequality and marginalization intersect, such as the self-organized refugee movement Refugee Struggle for Freedom that fights for rights and representation, and organizes hunger strikes and protest marches. There have been a number of protests in solidarity with refugee struggles in the UK, and a proliferation of grassroots activist efforts including transporting supplies from the UK to refugee camps in Calais such as Bikes without Borders. Experiences of mental illness do not have to be individualized or depoliticized, with organizations such as the Mental Health Resistance Network looking at wider political context of psychiatric care, and grassroots organizations forming to fill the gap left by government cuts to refugee mental health care.